Abstract
Purpose:
In 2016, Malawi implemented a universal test and treat (UTT) policy, expanding eligibility for antiretroviral therapy (ART) to anyone with confirmed HIV infection. Prior to 2016, Malawi restricted ART initiation to HIV-positive individuals with CD4 count ≤500 cells/µL, with WHO staging ≥III who were pregnant or breastfeeding, or who were younger than 5 years old. Here, we assess the impact on distribution of lymphoma presentation and baseline clinical characteristics at Kamuzu Central Hospital, Lilongwe, Malawi.
Methods:
Participants with newly diagnosed, pathologically confirmed lymphoproliferative disorders were enrolled from 2013 - 2020. We categorized participants as pre-universal ART (pre-UART) if enrolled during 2013-June 2016 or post-universal ART (post-UART) if enrolled during July 2016-2020 and evaluated clinical characteristics.
Findings:
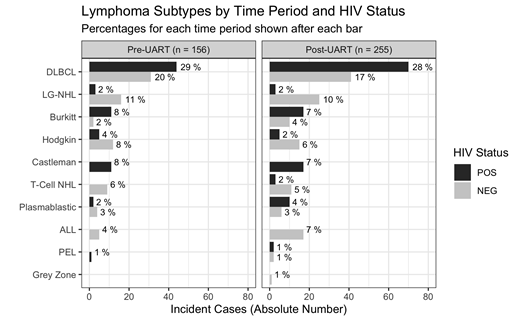
Of 412 total participants, 156 were pre-UART and 256 were post-UART. The most common diagnoses were diffuse large B-cell lymphoma (DLBCL) (45%), low-grade lymphoma (11%), Burkitt lymphoma (10%), Hodgkin lymphoma (9%), and multicentric Castleman disease (7%) and there was no significant difference in distribution of diagnoses between pre-UART and post-UART periods (Figure 1). HIV prevalence was 50%, mean age 43, and 62% male. Sixty-six percent (48/73) of pre-UART HIV-positive participants knew their HIV status, for median 5 years (IQR 2-8) and 71% (41/58) were on ART for median 4 years (IQR 2-7). Eighty percent (94/117) of post-UART HIV positive participants knew their HIV status (p=0.02), for median 4 years (IQR 2-9) and 84% (89/106) were on ART (p=0.05) for median 4 years (IQR 2-8). HIV was suppressed <1000 copies/mL in 56% (33/59) pre-UART and 71% (73/103) post-UART (p=0.05). Among DLBCL participants, 61% (23/38) of pre-UART HIV-positive participants knew their HIV status, for median 5 years (IQR 2-9), 61% (19/31) were on ART for median 4 years (IQR 2-6). Eighty-two percent (n=51/63) of post-UART DLBCL HIV-positive participants knew their HIV status (p=0.02) for median 5 years (IQR 2-9) and 89% (47/53) were on ART (p < 0.01) for median 5 years (IQR 2-9). Post-UART DLBCL participants had median HIV viral load of 0 log copies/mL (IQR 0-10) compared to pre-UART (6.2; IQR 0-10) (p=0.09). CD4 count, age adjusted-IPI and Ki67 proliferation index were similar for DLBCL patients in the two groups.
Interpretation:
There were no significant differences in lymphoma subtypes diagnosed or in traditional DLBCL prognostic factors after implementation of universal ART in Malawi. However, HIV was better controlled in the post-UART period and differences in immunological status may have implications for therapy and prognosis. Strengths of this study include a deeply characterized cohort, both clinically and pathologically. As opposed to epidemiological data from the US and Europe, we did not see a major shift in diagnoses over this time period with increasing access to ART. However, possible explanations for the differences include that this is not a epidemiological survey as cancer registration data is not comprehensively collected in Malawi and that the roll out of ART across sub-Saharan Africa has been much more gradual than the abrupt increase in access that was seen in the US and Europe. Therefore, epidemiological chances may also be more gradual. In summary, this is some of the most comprehensive data on lymphoma presentation from sub-Saharan Africa across periods of increasing access to ART and despite improved HIV control among incident lymphoma cases, there was no change in the distribution of diagnoses in this time period.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal